
The Trump The administration turned down a proposal from the Obama-Biden era that intended for Medicare and Medicaid to provide coverage for obesity treatments. drugs such as Ozempic and increase accessibility to these medications for millions of Americans.
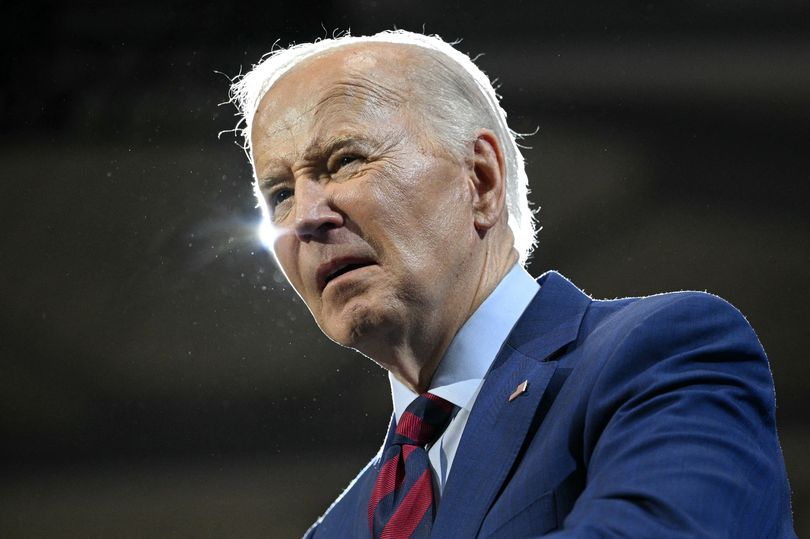
The announcement made on Friday dismantled the strategy put forth by the previous president. Joe Biden to reverse the legislation setting up Medicare's Part D prescription drug benefits, which prohibits the program from paying for medications marketed as "weight loss" aids.
The plan put forth by the Biden administration, crafted in November, aimed to circumvent the prohibition and include these medications within Medicare’s coverage. The administration contended that permitting access to these drugs could help address obesity and associated health issues.
READ MORE: Trump unveils 'pitiful' $5 million gold card featuring his image
READ MORE: Trump experiences a mental breakdown during his live Liberation address when he has a 'senile' moment onstage.

Increasing the scope of these drug coverages would have entailed significant expenses for the federal government. This led to the proposal becoming a focus for both the Trump administration and Elon Musk’s Department of Government Efficiency (DOGE). The department aimed at eliminating what they deemed as “inefficient” spending within governmental budgets.
The president contends that Biden's proposal would result in an utter squandering of billions in public money — according to the Biden administration’s estimates, this could amount to roughly $35 billion at the federal level over ten years, translating to approximately $3.5 billion annually if averaged out, although uncertainty remained regarding whether these figures were accurate.
The choice made on Friday was included in a substantial 438-page rule update that modifies certain aspects of the programs providing prescription drug benefits and private health care coverage for recipients. As per The New York Times report, this recent modification did not provide an explanation as to why Medicare should exclude these medications.
Catherine Howden, a spokesperson for the Centers for Medicare and Medicaid Services, informed the publication via email that the agency feels extending coverage currently “is not appropriate.” However, she noted that the possibility of covering these medications remains open, and they might explore potential future policies regarding them.
Medicare, the federal insurance program designed for seniors aged 65 and older as well as those with certain disabilities, indeed covers medications prescribed for diabetes patients and also includes a limited number of people dealing with both obesity and additional medical issues like cardiovascular disease or sleep apnea.
The Biden proposal aimed to extend coverage to individuals with obesity without including other medical conditions. According to estimates from Medicare administrators, approximately 3.4 million additional people might have opted for these medications under this new policy.
Robert F. Kennedy Jr., who recently took office as the head of the Department of Health and Human Services, has strongly criticized weight loss medications, asserting that adopting nutritious eating habits is far more effective than using such drugs.
Nevertheless, the medications demonstrated in clinical studies not only significant assistance with weight reduction but also provided additional advantages such as reducing the risk of heart attacks and strokes. Advocates supporting broader access emphasized these extra health benefits and contended that the investment made by the government towards covering these drugs would eventually offset its initial costs over time.
The advocates argued that patients would become more healthy, thereby preventing costly expenses associated with additional medical visits. However, it remains uncertain whether these potential cost savings will indeed come to fruition.
Medicaid programs at the state level, designed to offer medical care to those with low income, may decide whether they want to include the medication in their coverage, and numerous states opt to do so. However, had the wider-reaching Medicare rule come into effect as initially planned, all regions would have been obligated to provide this coverage.
Obesity medications can amount to several hundred dollars per patient monthly for programs like Medicare and Medicaid; however, the precise expenses remain unclear. Numerous employers along with various private health insurance providers do not include these drugs in their coverage. In fact, certain entities such as state employee benefit schemes in North Carolina and West Virginia discontinued covering these medicines following an increase in demand due to their significant expense.
Several Republican members of Congress have shown openness and enthusiasm about making Medicare cover the medication, though it isn’t considered a high-priority issue by many. It’s worth noting that this concept was apparently part of a roster of policy alternatives compiled by the House Budget Committee previously in the year.
What is the price range for weight loss medications?
Currently, Eli Lilly and Novo Nordisk, which are leading manufacturers of weight loss, obesity, and diabetes medications, charge patients between $350 to $500 per month if they choose to pay directly rather than using insurance coverage.
However, this represents a notable decrease compared to the expenses documented over the past few months, where costs occasionally surpassed $1,300 monthly. Consequently, individuals lacking coverage for these medications have allegedly turned to more affordable alternatives created via an ingredient-mixing procedure called compounding.
These versions were permitted due to a shortage of branded medications. Typically, they priced under $200 each month; however, authorities have instructed these sales to decrease gradually now that supplies of the branded drugs have been replenished.
